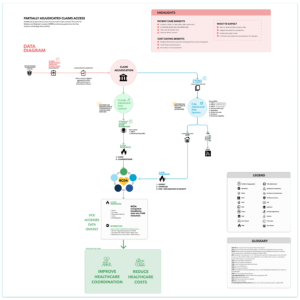
Services are rendered to someone with Medicare. After the care is given, the claim is submitted. A claim can be submitted up to a year from the service date. The detail to learn here is this is when the clock starts. The claim submission timeline begins here. Medicare Administrative Contractors, or MACs receive, validate, and aggregate the claim. This is where the claim data begins the adjudication process. The red circle is the System Software in CMS. The blue line illustrates fully adjudicated data. The green line shows partially adjudicated data. To be clear, these are not different data pathways. This just illustrates the timing of the available data. The data from claim submission to Common Working File (CWF) typically takes about 8-14 days. Here is where the customer can view claims in the final active stage. This means this is the first time customers can view adjudicated data. The data available that is fully adjudicated is
- PART A – Hospital Insurance
- PART B – Medical Insurance
- PART D – Drug Coverage
- Beneficiary Eligibility
- Deductibles
- Enrollment
- Historical Claims Data
- Lifetime Coverage
After the data is Fully Adjudicated, a small percentage of claims travel to the Integrated Data Repository IDR and then end in the Claims and Claims Line Feed File, CCLF. However, the majority of raw data becomes a single-line data source from the chronic condition warehouse. The data is then served to our customers in a standard format, which is the Fast Healthcare Interoperability Resources, known as FHIR “fire”. Referred to as models. What are Fast Healthcare Interoperability Resources? FHIR was developed by Health Level Seven or HL7. Health information can be exchanged between different computer systems regardless of how it is stored. It ensures that health information, including clinical and administrative data, can be accessed securely by those who need it, as well as by those who have the right to do so. Health Level Seven develops and updates FHIR in a collaborative manner. In FHIR, each model format is organized for displaying certain subsets of the raw claim data. At this point, you see the formats are
- Patient
- Coverage
- Explanation of Benefit
Customers accessing the data, go to one model or another depending on their goals. Now you see the arrow here going to this logo. This is the logo for Beneficiary Claims Data Application Programming Interface or BCDA. We’ll learn more about this in a minute. You can see here – partially adjudicated data updates. Here is where customers can view each step of the process of a claim in raw data in near-daily view. Users can see ‘snapshots’ of a claim. This is compared to the adjudicated claims where the user has to wait until the end of the adjudication process to see the data. The snapshots a customer can view of the data are Part A and Part B data – excluding Durable Medical Equipment (DME). These snapshots can be seen within 2-4 days of a claim submission. At the moment, our team is in Limited Launch. There are 4 Direct Contract Entities that are requesting data from our API. They can access partially adjudicated data. The data flows into FHIR, Fast Healthcare Interoperability Resources and from then is classified into two formats of data Claim and ClaimResponse. These two formats travel into BCDA. This is the view of what a user can access from BCDA. There are 5 models of data to choose from.
- PATIENT
- COVERAGE
- EXPLANATION OF BENEFIT
- CLAIM
- CLAIMRESPONSE
It’s important to note that the user doesn’t see “adjudicated” and “partially adjudicated data”. All they see is a buffet of resources. They choose each one depending on their needs.